*Person Collapses (Adult, assume cardiac arrest)
*Check Responsiveness and Breathing - simultaneously (Tap and Shout) "Are you okay?" - If unresponsive or if patient is not breathing or is agonal breathing, then
*Call emergency response system (call 911 or if in a medical setting call a code blue or retrieve a
defibrillator/AED if available) - the main rhythm associated with cardiac arrest in an adult is V.fib or
Pulseless V. Tach and NEEDS to be shocked as soon as possible to survive.
Begin BLS: Primary Survey
C-CIRCULATION (3 steps):
1. Check responsiveness and for breathing – Tap and shout, "Are you okay?”
Check responsiveness and for breathing – Tap and shout, "Are you okay?”
– look for chest rise – if no response or breathing or abnormal breathing
(agonal or gasping breathing) go to next step.
2. Call a Code Blue if in hospital or if out of hospital Call 9-1-1
Call a Code Blue if in hospital or if out of hospital Call 9-1-1
3. a. Check Circulation- by palpating a carotid/femoral pulse (5 no greater than
a. Check Circulation- by palpating a carotid/femoral pulse (5 no greater than
10 seconds). If no definite pulse within 10 seconds then, begin chest
compressions. If a definite pulse is felt, then give 1 breath every 6
seconds for adults, 1 breath every 2-3 secs for children and infants. Recheck
pulse every 2 minutes or 5 cycles.
b. Provide - CIRCULATION w/chest compressions and ventilations
(30:2) for at least 100-120 compressions per minute, “hard and fast”, at
least 2 inches deep with minimal interruptions. Allow for complete
recoil of the chest after each compression.
A-AIRWAY: Open the AIRWAY using head-tilt-chin lift, if trauma suspected, then use jaw thrust method. Infants need a neutral sniffing position. Even if trauma suspected and you are the only rescuer available, then open the airway using head-tilt-chin lift.
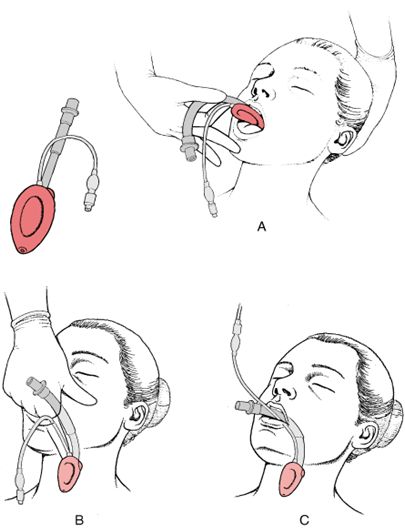
B- BREATHING: Assessment of this was done in step one - Provide BREATHING (2 breaths) allowing the chest to rise each time, give each breath over 1 second. Avoid excessive ventilations. If the breath does not go in, reposition the head by head-tilt-chin lift and attempt to deliver 2 breaths. Utilizing a bag-valve-mask (BVM) requires a good seal – E-C method, E with 3 fingers along jawbone and C with thumb and forefinger on the mask. Please note that this is best done with 2 rescuers and not recommended for the single lone rescuer.
Helps arrives and begins D for defibrillation, or if patient has a definite pulse, then skip to the secondary survey.
D=Defibrillation, Attach to a defibrillator-monitor or with paddles do a quick look for a shockable rhythm. We are looking for V.fib or pulseless V.Tach to defibrillate.
Secondary Assessment:
C=Circulation: Resume CPR with Chest Compressions 30:2; Start IV, Give Meds
A=Airway - Is the airway open and patent? If not, secure the an airway with an advanced airway device. Intubate patient with an ET tube or another advanced airway
(see below for different types and for a discussion on intubation)
Continuous waveform capnography is recommended as the
recommended secondary confirming technique and recommended for
maintaining correct placement of the endotracheal tube. Class I.
PETCO2 (partial pressure of end tidal carbon dioxide) normal range is
35-40 mmHg. If < 10 mmHg, in arrest, then improve the quality of
CPR.
B=Breathing - Are ventilation and oxygenation adequate? Place on oxygen and/or confirm placement with capnography. Once the advanced airway is in place. RR then should be 1 breath every 6 seconds (10 breaths per min) and NOT synchronized with chest compressions. If patient has a pulse and does NOT have an advanced airway, then ratio is 1 breath every 6 seconds for adults and 1 breath every 2-3 seconds for children and infants.
C=Circulation – Is CPR resumed with chest compressions? Has an (intravenous device) IV been placed? Antecubital vein is 1st choice for peripheral line/IO (intraosseous) route is an acceptable alternative and give medications (Vasopressor) - CPR for 5 cycles/2 minutes - meds (Antiarrhythmic). No interruptions from CPR for more than 10 seconds.
D=Determine the cause 5Hs and 5Ts and Disability - If get patient to ROSC (Return of Spontaneous Circulation). What is the patient's neurologic function? AVPU - Alert, Voice, Pain, Unresponsive; E=Exposure - Remove all clothing to access for any potential problem. SAMPLE=Signs and Symptoms, Allergies, Medications, Past medical history, Last meal eaten, Events (what happened) - look for 5 Hs and 5 Ts: Hypovolemia, Hypoxia, Hydrogen Ion (Acidosis), Hypo/hyperkalemia (low or high K level), Hypothermia, & Tension Pneumothorax, Tamponade-cardiac, Toxins (overdose - see PEA for tx), Thrombosis-pulmonary (Pulmonary Embolism-PE), Thrombosis-cardiac (Myocardial Infarction-MI).
A=Airway and Adjuncts
1. Oxygen is still recommended to be given at 100% to the unresponsive patient, but should be titrated down as soon as ROSC (Return of Spontaneous Circulation) to maintain sats > or = 94%.
2. Passive oxygen delivery or hands only Chest Compressions provide expelling air from the lungs and allows recoil of the chest which draws in air or oxygen. While there is promising data to show improvement in the out of hospital setting (utilizing a mask and 100% oxygen while chest compressions are done), the AHA does not recommend removing ventilations for the health care provider.
3. Bag-Mask Ventilations - best utilized with 2 persons and is not recommended for the lone rescuer. Provide an adult bag (1-2 Liters) and utilizing the head-tilt-chin-lift to pull the head into the mask obtaining a good seal deliver about 600 mL of volume or enough to cause chest rise over 1 second.
4. Cricoid Pressure - is NOT recommended for routine use during resuscitation to prevent gastric inflation. This is a change as it has always been recommended in the past. There have been mixed results: helping to stop gastric inflation, but many times impeding ventilation and even intubation.
5. Oropharyngeal Airways - can be helpful in maintaining an open airway in the unresponsive adult with a bag-valve-mask. The concern is that the if semi-conscious or if placed incorrectly, the patient's airway can be occluded by the oropharyngeal airway.
6. Nasopharyngeal Airways - are more helpful in the semi-conscious adult where the oropharyngeal airway cannot be placed to help with a bag-valve-mask to ventilate an arrested patient. The Circulation, part 8, article sites a study done in 1993 that assessed placement of nasopharyngeal airways that says bleeding may occur in as much as 30% of patients. It also reports 2 cases of inadvertent intracranial placement of the airways with patients with basilar skull fractures. Generally speaking, nasopharyngeal airways should not be placed into a patient with a basilar skull fracture, facial fractures, or bleeding disorders.
7. Advanced Airways - were once the gold standard for all arrest patients. There are recent studies that show delayed endotracheal intubation, passive oxygen delivery (O2 with hands only chest compressions) and minimally interrupted chest compressions was associated with improved neurologic survival.
A. Supraglottic Airways - There is no evidence that advanced airways improve survival rates in arrest situations out of the hospital setting. Direct visualization of the glottis is not required for these airways and therefore are easier to train and maintain skills in placement of these devices. It has been shown to be as effective as endotracheal intubation and the bag-valve-mask.
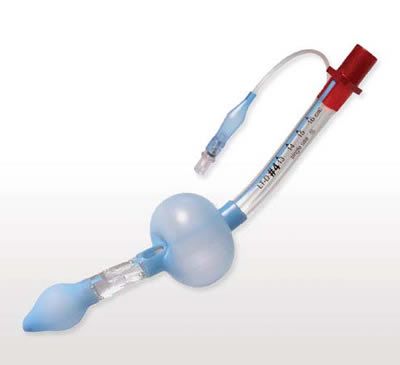
1. Esophageal-Tracheal Tubes (Combitube) - This
tube can be placed blindly into the esophagus or
into trachea just as an endotracheal tube (ET tube)
would be placed. The crucial part is to identify
where the tube is actually placed in order to
properly oxygenate and ventilate the patient. It requires
inflating two balloons and determining which tube is
ventilating the patient. Patients have died as a result
of ventilating the wrong tube. Quotations p. S732 provide statistics
on successful ventilation at 62-100% in different studies.
It can be used as an alternative to bag-mask ventilation or
endotracheal intubation.
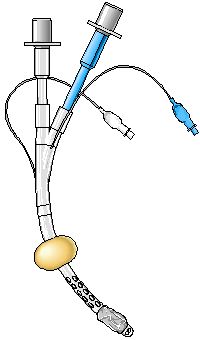
2. Laryngeal Tubes (Laryngeal Tube or King LT)
The King LT is a shorter tube with one tube, two balloons
and one valve, inflating one balloon blindly (meaning
one does not have to use a laryngoscope or see the vocal
chords) that should go into the esophagus.
The advantage over the Combitube is that one does not
have to spend the time trying to determine which balloon
should be inflated. Quotations p. S732 provide statistics
on successful ventilation at 85-97% in different studies.
It can be used as an alternative to bag-mask ventilation.
The picture is taken from http://www.sedationresource.com/
display-product/1-402-05/King-LT-D-Sz-5 without permission. If the owners
contact me, I will remove the picture.
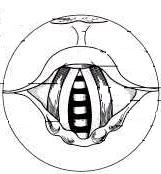
3. Laryngeal Mask Airways (LMAs)
LMAs are typically seen used in
shorter surgeries to avoid the potential
trauma to the vocal chords that an
Endotracheal (ET) tube would cause.
For some patients even with successful
placement, some cannot be ventilated.
Quotations p. S732 provide statistics
on successful ventilation at 72-97%.
It can be used as an alternative to
bag-mask ventilation or endotracheal
intubation.
http://www.merck.com/media/mmpe/figures
/figure1sec6ch64_eps.gif
B. Endotracheal Tubes
Once the gold standard for securing the airway, it is fallen a bit due to
complications, interruption of chest compressions, and lack of success in monitoring the placement. There is no evidence that out of hospital,
the ET tube is more advantageous than the bag-valve mask.
I'll discuss the laryngoscope and process of intubation.
*Intubation: ET Tube choice depends on the size of the individual. A general rule is to look at the patient's "pinky" finger for the diameter of tube to use. Generally, 7.0-8.0 for a woman and 8.0-9.0 for a man. Check the balloon with a 10 mL syringe by inflating the balloon, while still maintaining sterile in package. Put pressure on the inflated balloon, then deflate by withdrawing the 10 mL of air. Make sure suction is available to suction out the mouth. Then, choose the type of blade to use.
Straight blade (Miller Blade) - goes over the
epiglottis and exposes the glotic
opening visualizing the chords directly.
Also called a direct intubation.
Curved blade (Macintosh Blade) - goes into the
vallecula (the space between the epiglottis
and the tongue) and displaces the epiglottis
anteriorly as you lift up to visualize the vocal
chords (white upside down V like shape).
This is also referred to as an indirect
intubation.
Make sure your bulb is "white, tight, and bright." Many laryngoscopes are now fiberoptic and have no bulb. Older models would still have a bulb that could burn out or become loose and fall into the lungs if not tightened. Change batteries in the handle if needed. Do NOT provide cricoid pressure (Sellick's maneuver) with the thumb and fore finger to the cricoid cartilage (just below the "Adam's apple"). This is no longer recommended.
The goal is to place the endotracheal tube (ETT) or another advanced airway in the glotic opening of the Larynx; the balloon is to be just past the vocal chords (1-2cm past). Take no longer than 30 seconds to attempt to intubate. Note: NEVER, EVER, LET GO OF THE TUBE UNTIL IT IS SECURED.
Primary confirmation is direct visualization of the tube through the vocal chords and auscultation of the lung sounds, bilaterally and abdominal sounds in the epigastric area.
The secondary confirmation should be the continuous waveform capnography as the most reliable method of confirming and monitoring placement of the ET tube, p. S733.
The end-tidal CO2 detector (bag the patient 6 times at least then place the device on the ETT and it will turn yellow to indicate CO2 if it is in the trachea) can be used as a short term means to confirm placement if waveform monitoring is not available after visualization and auscultation.
The esophageal detector (squeezing the bulb once attached to the tube and then release - if in the trachea, the idea was that the cartilage around the trachea will allow the bulb to reinflate. But, if it was in the esophagus, it would not reinflate) can be used as a short term means to confirm placement if waveform monitoring is not available after visualization and auscultation.
The recommendation is 500-600mL of tidal volume will cause chest rise instead of the previous thought of 700-1000mL, but most importantly visible chest rise, since we wouldn't be measuring the tidal volume.